Old Photos
10/12/2025
Old picture when I used to drive 260 km between Austin San Antonio 3 times a week, I did this for years.

Mom when I started ClinZen new office in Hyderabad in 2013, I was still working in US and running it remotely

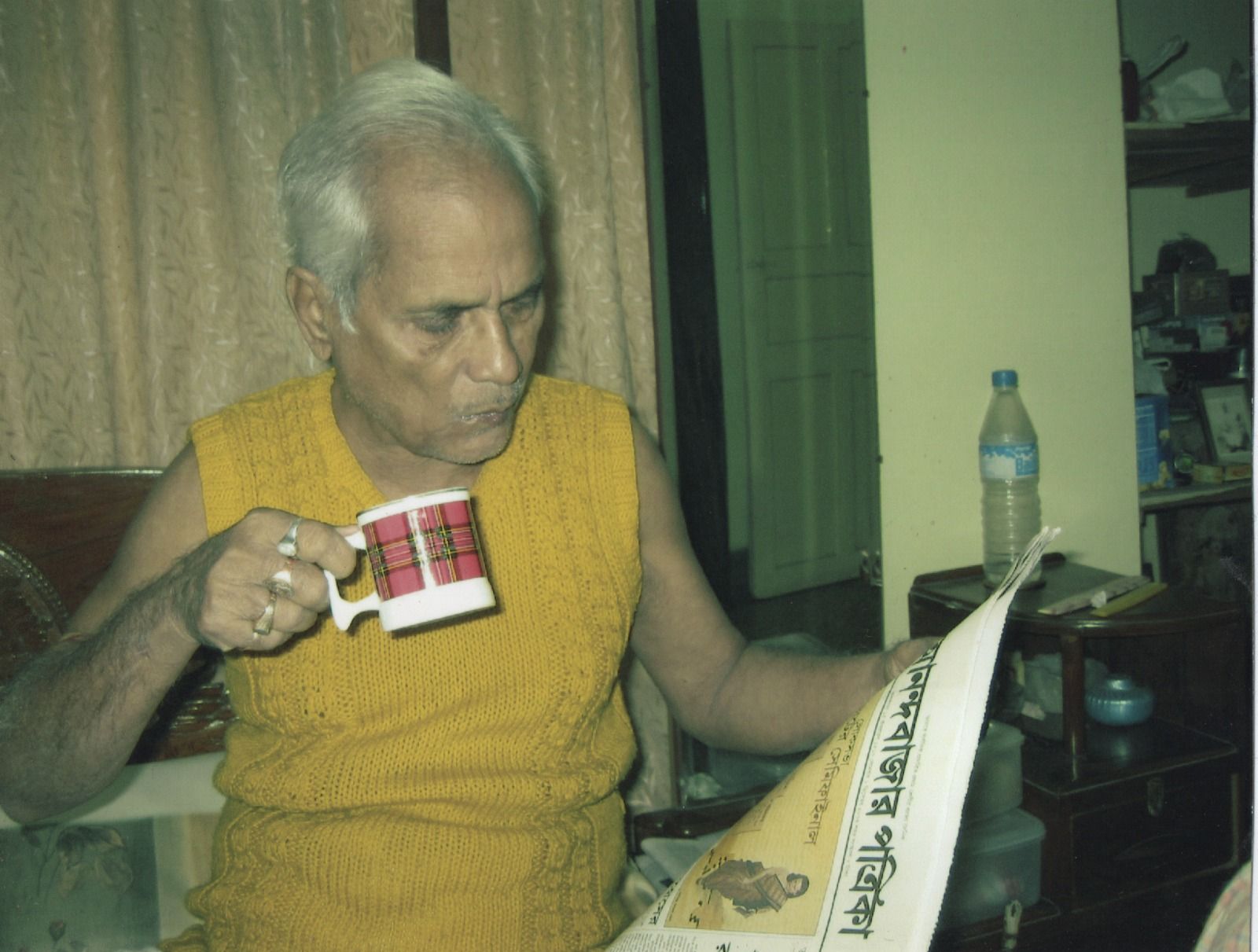
Old picture of my baba (father) who was alive when he was reading the newspaper, died of criminal medical negligence, in India hospitals don’t check for antibiotic resistance but keep guessing to give a MRSA bacteria time to kill, this and the movie Anand were why I had come back with a health information exchange plan with modernized hospital record systems and clinical trial management integration
The reason why antibiotic resistance is a problem in India is a long list, and if today I go to a hospital and I am unable to force the physician to do the right things, I will die. Let me at least make sure whoever reads this post doesn’t have to lose a person or himself/herself because of the assholes we have in buildings we think will cure us. If you don’t know this, you are FUCKED or DEAD.
A bacterial culture and sensitivity test is like sending a criminal sample to a forensic lab before you start arresting everyone in the neighborhood.
Here’s what actually happens. A bit of the infected material—blood, urine, pus, sputum, whatever—gets placed on a nutrient gel that encourages any bacteria present to grow. After 24 to 48 hours, you have colonies of the actual bacteria causing the infection, not just a guess. The lab then exposes these colonies to tiny discs of different antibiotics. Some antibiotics kill the bacteria in that dish; others don’t. The pattern that emerges tells doctors exactly which drug will work and which ones are useless.
Why that matters: without this test, prescribing antibiotics is guesswork. Doctors shoot in the dark. In India (and particularly Kolkata), decades of overprescription—antibiotics for viral fevers, sore throats, or even as a “precaution”—have trained bacteria to evolve resistance. It’s evolutionary natural selection, but sped up by human folly. The result is the rise of pathogens like MRSA, which laugh at most standard drugs. Every time an antibiotic is used unnecessarily, it wipes out sensitive bacteria but spares and strengthens the resistant ones, who then spread.
Culture and sensitivity testing interrupts that spiral. It’s like interrogating the culprit before deploying the entire army—it saves resources and prevents collateral damage. You discover whether the infection even is bacterial; if it’s viral (like influenza, dengue, or COVID), antibiotics do nothing except destroy your beneficial microbiome and create resistant strains.
Now, about microbiome casualties. Antibiotics are not snipers; they’re carpet bombers. They annihilate good bacteria in your gut, mouth, skin, and elsewhere—the invisible allies that digest food, synthesize vitamins, and keep pathogens in check. That’s why after antibiotic courses people often get diarrhea, bloating, or new infections like fungal overgrowth.
To restore balance, supplements matter—not as trendy wellness fluff, but as microbiological first aid. Probiotics (live beneficial bacteria like Lactobacillus or Bifidobacterium) and prebiotics (the fibers those bacteria eat) help repopulate your gut. Zinc, vitamin D, and certain amino acids help the immune system recover. A diverse, plant-rich diet feeds the right microbes back into balance.
Make fucking sure of these or die:
Culture first tells you if antibiotics are needed at all, and which one.
Judicious antibiotic use prevents resistance and preserves future drug power.
Microbiome support afterward prevents collateral damage and strengthens recovery.
Skipping the culture test and pumping antibiotics into a population that already overuses them is like trying to fix a leaky pipe with a flood—it makes the problem worse, just more spectacularly.
These are the all the reasons, and paraphernalia of jargon to be aware of (from research publications):
high MRSA prevalence in tertiary hospitals, unregulated antibiotic use in community and hospitals, inadequate hand hygiene compliance, poor infection control and sterilization practices, nursing shortages and excessive workload, overcrowded wards and high patient density, delayed microbiology culture and sensitivity reporting, inappropriate empiric antibiotic therapy, limited access to MRSA-effective drugs, multidrug resistant MRSA strains, elderly immunosenescence and frailty, multiple chronic diseases (diabetes, CKD, COPD, heart disease), malnutrition and low protein levels in elderly, invasive devices (catheters, IV lines, ventilators), long hospital stays increasing exposure, poor hospital housekeeping and surface disinfection, lack of infectious disease specialist oversight, insufficient antimicrobial stewardship programs, poor adherence to infection-prevention checklists, inadequate AMR surveillance at facility level, high healthcare worker MRSA colonization, delayed recognition and management of sepsis, device-associated bloodstream and respiratory infections, polymicrobial infections complicating therapy, poor sanitation and environmental hygiene, overcrowded emergency and inpatient facilities, socioeconomic deprivation delaying treatment, poor public health funding and infrastructure, limited diagnostic capacity and outdated labs, weak hospital administration accountability, inadequate training and refreshers for clinical and cleaning staff, burnout among healthcare workers, weak antibiotic policy enforcement, poor nursing supervision and patient monitoring, lack of isolation or cohorting for MRSA cases, insufficient availability of PPE and compliance lapses, poor waste segregation and biohazard management, under-resourced ICUs and geriatric wards, inconsistent infection control audits, lack of rapid diagnostic tools, poor post-discharge follow-up, weak rehabilitation and long-term care pathways, insufficient community awareness about infection prevention, high background disease burden in Kolkata’s elderly population, inadequate integration with national AMR programs, poor data collection and feedback mechanisms, reuse of medical disposables, contaminated hospital environment, poor record keeping and reporting, deficient ventilation and overcrowded infrastructure, weak enforcement of pharmacy regulations, antibiotic self-medication, poor dietary quality among elderly, socioeconomic inequality, weak referral and continuity-of-care systems, limited hospital epidemiology expertise, lack of motivation and accountability in infection control teams, insufficient cleaning supervision, overall systemic neglect of infection prevention and control.